1 Supporting Excellence in Interdisciplinary Research


I’m excited that DLSPH is creating new structures to enable truly interdisciplinary and cross-disciplinary research. This is helping me to collaborate with the wide range of experts I need to help bring precision public health into practice.
The research engine at DLSPH is continuing to move at high speed, with increased research support for faculty and funding opportunities and successes that include but go beyond COVID-19, which is the prominent research concern of the year globally and is addressed elsewhere in this report.
In addition to creating seed funding for COVID-19 research in March, DLSPH set aside seed funding for non-COVID-19 research to preserve the richness of the School’s research portfolio through prioritization of non-COVID-19 research proposals.
The Office of Research continues to explore additional sources of funding. For example, DLSPH has provided $8,000 in seed funding for a grant to associate professor Aviv Shachak entitled Physician Burnout and Use of Mobile Information and Communication Technology, which will explore questions such as how and in what ways physicians engage with MICT for clinical and administrative work-related purposes outside of working hours.
DLSPH Office of Research
DLSPH faculty members have been very successful in obtaining funding for DLSPH-led studies, which has, in turn, led to an expansion of the support the research office can provide.
The increased funding, said Professor France Gagnon, Associate Dean – Research, has brought two new Canada Research Chairs (CRCs) to our school: a CIHR Tier 2 position, which was advertised in the fall of 2020, and a Tier 1 CRC, which will be advertised early in 2021. In addition, the influx of the number of research grants and grant funds has made it necessary to add a new research funding officer, Sarah Namer, to the staff. Namer came on board during the 2020-21 academic year and will support interdisciplinary research at DLSPH, as well as faculty award nominations. She works closely with Caroline Godbout, the research development officer, to support our researchers in their grant and award applications.
SSHRC Success
DLSPH researchers are claiming an increasing presence in social science research, with a tripling of funds from the Social Sciences and Humanities Research Council (SSHRC) in the past few years.
“We are very excited about the success of our principal investigators in the social sciences,” said Lee Vernich, DLSPH’s Director of Research. “Their success with SSHRC funding in recent years is particularly remarkable: our researchers have received more funding in the first three months of 2020 than in 2019.”
Five DLSPH researchers – associate professor Erica Di Ruggiero and assistant professors Meena Andiappan, Arif Jetha, Amaya Perez-Brumer and Jay Shaw — claimed success in the January 2020 Insight Development Competition, reflecting a strategy by the School to provide comprehensive research support to all faculty members. This resulted in increased participation by our School’s social science researchers in these competitions, allowing DLSPH to take advantage of SSHRC’s decision to fund health-related research.
Di Ruggiero will use the funds to study how political, social, cultural and economic factors are influencing Canada’s progress on implementing the UN’s 17 Sustainable Development Goals, while Jetha will study the unique challenges and opportunities for diverse groups of young people in the future of work. Andiappan is exploring the impact of workplace-required necessary evils — tasks in which a person must knowingly and intentionally cause emotional or physical harm to another human being in the service of achieving some perceived greater good — on unethical behaviour.
A number of these project are collaborative and/or interdisciplinary. Shaw, for example, is working with DLSPH colleagues Jennifer Gibson, director of the Joint Centre for Bioethics, and Alison Paprica of IHPME to explore the values that may be overlooked — such as equity and informed consent — when integrating Artificial Intelligence (AI) technologies into health care.
Meanwhile, Perez-Brumer will study the experiences of Venezuelan transgender women relocating to Peru, along with a multinational collaborator at U of T, the Universidad Peruana Cayetano Heredia and Féminas (a Peruvian transgender activist organization).
In addition, assistant professor Angela Mashford-Pringle, associate director of the Waakebiness-Bryce Institute for Indigenous Health, is immersed in the research funded by her 2019 SSHRC Insight grant that actually began in spring 2020. The project, entitled Kijibashik: Turn It Around―Indigenous Women’s Stories on Motherhood and Incarceration, is being conducted in partnership with Jerry Flores, an assistant professor of sociology at U of T
Interdisciplinary Research Areas
The DLSPH interdisciplinary research areas are new initiatives to foster collaboration across the School, the University, and beyond, on research and education efforts aligned with DLSPH research priority themes. With an injection of funding and planning support, the goal is to create new teams that are positioned for discovery and prepared to pursue the “big questions.” Their work will be used to help train the next generation of public health and health system leaders.
This past year, DLSPH invested in two teams to build the first interdisciplinary clusters over the subsequent three years:
The Data Science research cluster, led by associate professor Laura Rosella, is providing leadership in AI and emerging informatics and analytics technologies to improve population health and health systems performance. With 25 members from across nine divisions, the interdisciplinary team is leading important debates, training, and providing support for high impact data science research projects in population health. Its seed funding program for novel data science population health projects leveraged new priority funding from the Edwin S.H. Leong Centre for Healthy Children. In January, the cluster will hold the first of its public Conversations in AI and Health, a series that seeks to foster critical thought and debate regarding data science in the context of public health and health systems.
The Interdisciplinary cluster in Global Public Health and Health Systems Improvement through Implementation Science is co-led by associate professors Erica Di Ruggiero and Xiaolin Wei. It engages faculty and students from across the School, the University, affiliated hospitals and research centres, as well as faculty based abroad (currently including Kenya, the Philippines and Israel).
The team is building capacity in implementation science within and beyond DLSPH. Two new postdoctoral fellows have been engaged to develop projects that address different implementation science priorities, and more than 20 graduate students, in teams drawn from across DLSPH divisions and institutes, has launched group projects, co-mentored by cluster faculty members.
In a partnership with the WHO’s Special Programme for Research and Training in Tropical Diseases, the team will be piloting an international training program in Operational Research, involving expert facilitators with learners from Canada and low-and middle-income countries to develop actionable health systems research projects.
A third emerging research cluster, still in the formative stages, will focus on integrated care, in support of the DLSPH goal of “Building sustainable and equitable health systems through integration and engagement at the organizational, local and jurisdictional level,” and will draw inspiration from WHO reports on person-centred integrated care. Two inaugural meetings are scheduled for January 2021.
Professor Walter Wodchis will lead this initiative; the group’s vision is to achieve a person-centred sustainable, equitable, and integrated learning health system, drawing upon the expertise of DLSPH faculty and experts from across the university in five specific areas:
- Community-oriented care systems;
- Intersection between medical and social care;
- Organisational learning and innovation culture;
- Financing, economics and payment; and
- Digital health.
2 Building a Life-cycle of Cutting-edge Programming


Assistant Prof. Emily Seto, IHPME
Our DSLPH faculty members are in a unique position to provide cutting-edge educational offerings through their novel work in advancing digital health innovations. I’m excited to be part of the evolving programming at DLSPH that will help enable learners to be leaders in creating and implementing these new technologies.
Our School community has identified lifelong learning as a priority offering to our alumni. Staff and faculty are working to ensure that once a student earns a degree and takes a job in the field, there are excellent opportunities to build on their knowledge and chances to learn about the hot topics in public health. There are a number of relevant efforts underway at DLPSH, and there will be more to follow in the coming years.
The New DrPH Program
In May, Dean Adalsteinn Brown announced the creation of a new doctoral program at DLSPH: the Doctor of Public Health or DrPH. The program breaks fresh ground in the field of public health education by preparing public health professionals to lead change locally and globally. The program focuses on accelerating the use of research evidence to inform practice and policy. Students develop and advance important key leadership, management, and public health practice competencies. The program began in September 2021 under the leadership of Erica Di Ruggiero, an associate professor and director of the Centre for Global Health.
IHPME’s AI in Health Certificate
The Institute of Health Policy, Management and Evaluation (IHPME) is home to most of DLSPH’s education initiatives, including continuing education programs that offer health professionals the opportunity to stay current with the latest developments in the field and to acquire new skills. The Institute is a champion of forward-thinking programming, as illustrated by its launch earlier this year of a flagship program in what will be a series of opportunities to bring Artificial Intelligence (AI) into the health sector: the AI in Health Certificate.
The new certificate, created by Assoc. Prof. Emily Seto and Asst. Prof. Julia Zarb with input from an advisory board, will prepare health-care professionals to apply innovations in AI for health generally, while allowing them to tailor AI to their own organizations through project work. Modules for the AI in Health Certificate cover a wide range of topic areas, including ethics and policy and AI in health strategies, business cases and data and information governance. DLSPH faculty and expert instructors working in the field of AI teach the course modules.
“The content is rooted in an in-depth understanding of health care systems and implementation science, and addresses the essential ethical issues that practitioners need to understand to deploy and manage AI in socially responsible ways,” says Eric Shaw, an assistant professor at IHPME and a senior scientist at the Women’s College Hospital.
Modernizing Graduate Education
Taking courses online is a necessity during the pandemic, but it can sometimes be challenging. Luckily, Angela Mashford-Pringle, the associate director of DLSPH’s Waakebiness-Bryce Institute for Indigenous Health, who teaches a ground-breaking land-based learning course, isn’t afraid of a challenge.
Initially, Mashford-Pringle didn’t think a course built around an Indigenous connection to the land could work remotely, but she created a format that made the course a success, despite the absence of the usual week-long stay at U of T’s Hart House farm. Her revamped course includes lots of holistic, community-building discussion, but also an increased emphasis on each student’s personal relationship with the land they live on.
“Here’s something I worked very hard to put on the land and then I had to make it virtual — but it worked,” says Mashford-Pringle with pleasure. “I was shocked in a good way.”
3 Creating Impact from Our Work

Implementation science is playing a central role for health professionals to understand and identify ways to combat COVID-19. At the Institute for Pandemics, we’re producing control guidelines for health care workers in low- and middle-income countries. I’m excited to see DLSPH take a leadership role in this area.
Knowledge creation is a large part of the work done at DLSPH, but for that work to have an impact, it must travel beyond the borders of the classroom and into the wider world. In addition, DLSPH has a role to play in exploring and exposing gaps in the public health system or public health issues that deserve broader attention.
Teaching Journalism as a Public Health Tool
The opportunity to shape the public debate about health draws professionals and researchers to the Dalla Lana Fellowship in Global Journalism and its Certificate in Health Impact. These two programs, under the direction of Robert Steiner, teach graduate students, professionals and researchers how to work as reporters and how to deploy journalism as a public health tool.
In 2019-20, DLSPH added another important arm to its journalism program: The Investigative Journalism Bureau (IJB).
The IJB is led by award-winning investigative Robert Cribb, who has been teaching in the fellowship program since its inception in 2012, and is supported financially by Toronto business executive Gerry Gotfrit. The bureau will offer students throughout the university and worldwide the opportunity to work as investigative journalists in practicums or internships, collaborating on long-term projects over the course of a semester. It’s an opportunity for students at all levels to learn valuable journalism skills on the job, conducting document searches, submitting access-to-information requests and interviewing subjects.
The work done by the IJB provide DLSPH with another means of having public impact on important issues shaping the health of Canadians and amplify the public conversation around long-term public health strategies, such as youth mental health.
“Over the past decade, we’ve pioneered the process of quickly turning subject-matter specialists into journalists who can break important news in their own fields. This is the next step: turning them into investigative reporters,” says Steiner, who is also an assistant professor, Clinical Public Health and Institute of Health Policy, Management and Evaluation. “When subject-matter specialists start working as investigative journalists, democracy has a powerful new tool.”
IJB plans to follow its inaugural mental health series of stories with half a dozen new collaborative projects in 2021.
Launching the Institute for Pandemics
With COVID-19 cases skyrocketing worldwide, now is the time to think more broadly about pandemics. The DLSPH’s new Institute for Pandemics, created in August 2020 under the direction of Dean Adalsteinn Brown, is the world’s first academic centre dedicated exclusively to preventing, preparing for, fighting and recovering from pandemics.
The institute is part of an effort by the U of T to ramp up pandemic research and training for public health professionals, who can move quickly to implement evidence-based plans to prevent and control new infectious diseases.
“COVID-19 has exposed the limits of government and world bodies in detecting and responding quickly to emerging global disease threats,” says Brown, founding director of the institute.
“Universities have the range of expertise, the freedom to move quickly, the credibility of political neutrality and a duty to work closely with governments and other institutions to effectively respond.”
The institute draws on the expertise of world-class faculty from across DLSPH and the wider university to bring their expertise in fields such as infectious disease modelling, epidemiology and social determinants of health to bear on one of the recurring crises of modern times. It was launched with a $1 million gift from the Toronto-based Vohra-Miller Foundation.
Partnering With the World Bank
During the pandemic, DLSPH faculty and students have sought opportunities to positively impact health systems around the world. IHPME’s North American Observatory (NAO) partnered with the World Bank to analyze the COVID policy interventions of 10 countries in Latin America and the Caribbean, comparing them to the responses of South Korea and Uruguay. The study identified ways that countries could improve their responses to the pandemic and prepare for future health crises.
“The research team at NAO delivered rigorous and meaningful analysis to a dozen countries by working closely with World Bank staff and government counterparts to understand their contexts, compare and contrast their policy response and derive practical recommendations that are proving useful as governments face an acceleration of infections in early 2021” said Jeremy Veillard, Senior Health Specialist at the World Bank and Assistant Professor at IHPME.
Offering Free Public Programming
Sharing our expertise with the health-care community and the public is another way for DLSPH faculty members to share their thought leadership and impact policy. Throughout the year, DLSPH experts offer lectures about their areas of specialty. The School also invites experts on individual topics to visit DLSPH and offer the benefit of their knowledge to our students, faculty and staff. During the 2019-20 academic year, DLSPH offered the following opportunities, many of them focusing on issues related to the pandemic:
- Collaborative Specialization in Women’s Health Student Seminar Series. Held monthly at Women’s College Hospital.
- Doctoral Seminar Series in Epidemiology. A lecture series held twice a month on Thursdays, featuring faculty members and other practising epidemiologists.
- International Speaker Seminar Series. A lecture series held on the last Friday of the month.
- Joint Centre for Bioethics Seminar Series. A weekly series addressing a variety of bioethics topics.
- Strategic Training for Advanced Epidemiology (STAGE) International Speaker Seminar Series. Held on the last Friday of the month with support from the Canadian Statistical Sciences Institute (CANSSI).
- Other Research Seminars. Generally offered in collaboration with teaching hospitals or other departments within the University or the Faculty of Medicine:
Students at DLSPH also contributed to dissemination of knowledge by mounting a conference of their own that focused on altering our view of mental health. Shifting the Paradigm brought together voices from academia, social services, healthcare, policy and individuals with lived experience to share their insights.
As well this year, DLSPH’s Waakebiness-Bryce Institute for Indigenous Health (WBIIH) launched the Turtle Island Journal of Indigenous Health. The student-led journal is open access and peer reviewed. It’s mission is to foster respectful collaboration and the co-creation of knowledge within the field of Indigenous health, and to provide a forum for dialogue and knowledge translation between academia, Indigenous communities and broader society in a way that honours all Indigenous ways of knowing.
4 Global Health


I am honoured to be leading our School’s Centre for Global Health, an interdisciplinary hub that brings together faculty and students to co-design and implement novel research and education initiatives with impact on health systems and health equity globally.
To provide more cohesion for global health endeavours and make a greater impact in this field, in February 2020, DLSPH launched the Centre for Global Health as a global presence through collaborative research and education.
Centre for Global Health
Creation of the Centre for Global Health fulfilled a major goal of DLSPH’s 2019-2024 Academic Plan. A working group that was chaired by Erica Di Ruggiero, the Centre’s first director; and involved faculty and staff, shaped its vision as “an interdisciplinary knowledge hub that catalyzes excellence in global health research, education and service, and prepares future public health system leaders to make a global societal impact.”
The Centre offers interdisciplinary graduate education and continuing education, provides student practicums and develops partnerships with global health programs and experts worldwide. It will be home to speaker series, lectures and varied career and training opportunities, as well as a base for visiting global health scholars.
Through the catalytic work of Centre for Global Health, the DLSPH community is well-positioned to generate new knowledge to strengthen equitable health systems globally, and prepare system leaders to make a global impact,” says Di Ruggiero, who is also an associate professor of global health at DLSPH.
The first strategic initiative being undertaken by the Centre for Global Health is a major research and education effort in universal health coverage in line with the United Nation’s 2030 Sustainable Development Goals.
Executive Course in Global Health Diplomacy
The Centre for Global Health burst onto the scene with the introduction of its Executive Course on Global Health Diplomacy, a course designed to offer public health and other professionals an in-depth understanding of how the world of diplomatic negotiations works. By understanding global health diplomacy, both researcher and policymakers gain valuable insight into impacting health policy at the global level.
“There’s a lot of competition for ideas on the geopolitical stage,” says Professor Erica Di Ruggiero, director of the Centre for Global Health and co-founder of the course. “How do you get an idea on the agenda so that it sticks?”
Co-led by Erica Di Ruggiero and Garry Aslanyan with support from Centre manager, Ophelia Michaelides, this executive course is being offered in partnership with the Office of International Affairs for the Health Portfolio (Government of Canada) and the Graduate Institute of Geneva to 25 learners. The course is delivered remotely.
Inaugural Distinguished Visiting Global Health Leader
As outlined in the Academic plan, the DLSPH has begun to host senior global health leaders and executives in residence.
Professor Ilona Kickbusch, the founding director and chair of the Global Health Centre at the Graduate Institute of International and Development Studies in Geneva, is the Centre for Global Health’s first Distinguished Visiting Global Health Leader. Kickbusch’s breadth of experience includes serving as the inaugural head of Global Health Program at the Yale School of Public Health and a seven-year term at the World Health Organization.
Professor Kickbusch is sharing her knowledge of global health diplomacy with faculty and students, including mentoring students and assisting the Centre with national and global outreach and strategy development. She also advises on potential global health policies, partnerships and development opportunities.
Renewed Partnership With Moi University, Kenya
Given the fruitful collaboration between DLSPH and Moi University School of Public Health in Kenya that began in 2017, a second Memorandum of Understanding has extended the for five additional years, until 2025. The partnership is focused on collaborative public health education, research and capacity building initiatives that address implementation science, universal health coverage, knowledge mobilization and translation, and leadership. Erica Di Ruggiero serves as the Centre’s lead and associate professor Paula Braitstein is the faculty lead.
Specific objectives for the collaboration include:
- Initiating joint DLSPH-MUSPH research into achieving UHC in sub-Saharan Africa;
- Undertaking joint research in strategic areas;
- Increasing capacity of faculty, students, and county government officials in relevant areas to use implementation science; and
- Building capacity among government, students, and faculty to better use evidence to inform decision-making and to strengthen data collection.
“We are thrilled and delighted to be expanding upon the foundational work done to date,” says Braitstein, an associate professor affiliated with the Centre for Global Health. “We have launched several collaborative research, education and knowledge translation initiatives involving faculty and students from both schools, and are pleased with the progress thus far. We look forward to building on these important steps and are excited about the potential impacts.”
5 Equity


“There’s a lot of folks doing amazing Black health work at U of T and other places. I’d like to invite them to be part of what we’re creating!”
This past year at the DLSPH, we invested in further diversifying our faculty to strengthen our interdisciplinary research, and to make our teaching and community outreach efforts more relevant. By fostering a more inclusive workforce, we are better positioned to promote meaningful, sustainable public health solutions that achieve global impact.
Health Leads
This year, the School approved the addition of four new health leads in areas that are not regularly the focus of research or teaching: Black health, Indigenous health, LGBTQ health and women’s health. The first posting, for the Black health lead, was finalized in December 2020, and the others followed in 2021. These faculty members lead the development of an inclusive public health educational environment and ensuring that issues of equity and inclusion are woven throughout all aspects of our educational and research offerings. Learn more about the health leads on the Equity page of DLSPH’s website.
In the Works
DLSPH is also preparing to hire an assistant professor trained in Indigenous health for a position focusing on spinal cord and traumatic brain injuries. The position is a five-year term appointment and the successful candidate will be eligible to be appointed to the Professorship of Praxis Spinal Cord Institute and Ontario Neurotrauma Foundation Professorship in Indigenous Spinal Cord Injury and Traumatic Brain Injury.
New Faculty
Among those who joined our faculty this year is globally accomplished health systems and health economics researcher Dr. Beverley Essue, who studies barriers to equitable and affordable health care, particularly those faced by socioeconomically disadvantaged communities.
Prior to joining our Institute of Health Policy, Management and Evaluation (IHPME) in November, the U of T graduate (Hons BSc, 2002) built her credentials in Australia, earning a Master of Public Health degree and a PhD in Health Economics and Health Policy from the University of Sydney. For her doctoral research, Essue sought to understand the household economic burdens associated with chronic conditions: how do Australians afford out-of-pocket health-care costs, and how can social and health policies mitigate these costs? She later examined this same issue in Vietnam, which spurred her to align with the movement for universal health coverage.
After returning to Canada in 2015, Essue joined the Canadian Partnership Against Cancer to focus on enhancing Ontario’s cancer control system. She has also conducted research for Disease Control Priorities, a global multi-stakeholder public health initiative particularly focused on low-income countries; the Lancet Taskforce on non-communicable diseases and economics; and currently, the Lancet Commission on Gender-Based Violence and Maltreatment of Young People. At the IHPME, Essue is studying how to support effective health-care priority setting.
Dr. Roberta K. Timothy (PhD, adult education, 2007) an interdisciplinary scholar and health practitioner who specializes in the intersectionality of health, race and human rights, does research that aligns with our values promoting equity and social responsibility in health care systems.
As DLSPH’s new Director of Health Promotion, Timothy, an assistant professor in the teaching stream, brings a deep understanding of the unequal impact of social determinants of health across diverse local and global communities. For more than 30 years, she has studied and worked to address anti-Black racism and colonialism in community-based health promotion, policy and practice. She has extensive teaching experience in universities, colleges, social service organizations and community settings. For the last decade, she has run Continuing Healing Consultants, where she providers anti-oppression psychotherapy consultation and training.
At DLSPH, Timothy is studying two key themes in public health: criminalization and social determinants of health in African/Black and Indigenous communities; and mobilizing critical intersectionality and anti-oppression psychotherapy in community mental health. She is currently working on a two-year research project called “Black Health Matters: National and Transnational COVID-19 Impact, Resistance, and Intervention Strategies.” She prioritizes critical and creative approaches to knowledge production that reflect the experiences and aspirations of migrant, refugee, African/Black diasporic and transnational Indigenous communities. Recently, she has also spoken about the inequalities brought to the forefront by the pandemic.
The recent appointment of professor Janet Smylie as the Tier 1 Canada Research Chair in Indigenous Health, will help us better understand and address the complex factors causing systemic anti-Indigenous racism in health care.
A Métis physician who has practised family medicine in urban, rural and remote settings for 25 years, Smylie has directly observed how First Peoples in Canada receive second-class health-care service as a result of culturally insensitive practice approaches. She has undertaken many efforts to bridge these gaps, key among them working with First Nations elders to develop and direct Well Living House, a St. Michaels’ Hospital research centre focused on Indigenous infant, child and family health and well-being.
Through the CIHR-funded initiative Our Health Counts, she studies how social determinants of health such as housing, poverty, history of colonization and culture affect the health care of Indigenous people living in Ontario cities. Smylie’s research and advocacy have also influenced federal funding investments in Indigenous midwifery.
Smylie’s objective at the DLSPH is to advance Indigenous models, standards, tools and capacities for the planning, delivery and quality improvement of health services for First Nations, Inuit and Métis people. She is currently working on a project that aims to count the number of Indigenous people who have been infected, been hospitalized or have died from COVID-19.
In addition to more inclusive faculty appointments, during the 2019-20 academic year, the DLSPH launched a review of the School’s equity and inclusion climate. As the Black Lives Matter movement came to the forefront of public consciousness in 2020 with the increased visibility of police brutality, Dean Brown made a statement on the links between anti-Black racism and public health outcomes.
Indigenizing Our Physical Spaces
Thanks to the faculty and students at the Waakebiness-Bryce Institute for Indigenous Health, there is now a WBIIH Student Medicine Garden planted outside DLSPH’s home at 155 College St. WBIIH community members planted traditional bushes and other plants, including sage, tobacco and sweetgrass, and the garden is thriving.
6 COVID-19

The pandemic has demonstrated the crucial importance of public health schools as bridges between the academic research community, public health practice and government policy. DLSPH has been a global leader in generating the data and high-quality advice that decision-makers need.
In March 2020, it became clear that the novel coronavirus 19 was quickly assuming pandemic proportions worldwide. As public health and health systems experts, the faculty and researchers at DLSPH had a profound impact on the Canadian response to COVID-19, as modellers, policy advisors and trusted voices in the media. DLSPH faculty members experienced a 1,000 percent increase in media mentions compared to the same period in 2019.
Science Table: COVID-19 Advisory for Ontario
The Ontario COVID-19 Science Advisory Table, convened by DLSPH, is a group of volunteer scientific experts and health system leaders who evaluate and report on emerging evidence relevant to the COVID-19 pandemic, to inform Ontario’s response.
The Science Table, co-chaired by Dean Adalsteinn Brown of DLSPH and Brian Schwartz, vice-president of Public Health Ontario and a DLSPH associate professor, provide frequent summaries of relevant scientific evidence for the COVID-19 Health Command Table of the Province of Ontario, integrating information from existing scientific tables, Ontario’s universities and agencies, and the best global evidence.
The Science Table’s membership includes many DLSPH experts in their fields.
DLSPH Play Key Roles at COVID-19 Tables
Professor Jennifer Gibson, a respected bioethicist and director of DLSPH’s Joint Centre for Bioethics, became one of the Ontario government’s main bioethics advisors as the COVID-19 crisis unfolded. Gibson sat on five of the provincial pandemic advisory tables, created a sixth, the Bioethics Table, and co-chaired a seventh, the Critical Care Command Table. She was also a member of Ontario’s testing and health integration task forces. Especially in March and April, as the challenges of the pandemic became clearer, much of her time was devoted to the pandemic response.
“We’d done research on pandemics after SARS, but there’s nothing like being immersed in the real thing for revealing what you don’t know and must learn quickly,” Gibson says.
Both with the early PPE shortages and later, as the infection numbers grew, Gibson and her bioethics colleagues made recommendations on ethical priority setting and assisted decision-makers in creating an ethical triaged approach to critical care. She also developed bioethics briefs to frame issues such as the transfer of long-term care patients and closing down elective surgeries, which informed the decisions made by Ontario’s chief medical officer of health.
“This has been a voyage of discovery for all of us,” Gibson says. “We filled in a gap and now the good practices that have been developed can be brought forward to address other crises.”
Gibson noted that the experience has also been a wake-up call to health-care and to bioethics in terms of equity.
“The conversation has shifted,” she says. “Bioethics as a field has been very white and doesn’t engage with social determinants of health in practice. What was invisible has become very visible and we need to take stock.”
Leading U of T’s COVID-19 Response
The COVID-19 crisis led Professor Vivek Goel, U of T’s Vice-President, Research and Innovation, and Strategic Initiatives, to take on a new leadership role as Special Advisor to the President and Provost, guiding the university’s COVID-19 planning efforts.
Goel, a professor at DLSPH’s Institute for Health Policy, Management and Evaluation, says the pandemic was a call to action. As a public health physician, founding President and CEO of Public Health Ontario, Goel was uniquely qualified to contribute to public health policy and practice at a critically important juncture.
As the pandemic exploded, Goel was able to apply his remarkable expertise and experience to important discussions, locally, provincially and nationally, with considerable benefits to the University of Toronto and the province. From the outset, Goel was among the first to advocate for a shift toward a “population health model” when tackling the pandemic – one that would take into account the ways that lockdown can erode economic, social, and physical wellbeing.
To educate the public as the pandemic continued to cause uncertainty across the country, Goel launched a podcast on the topic – just one of the many ways he has shared his knowledge with those beyond the U of T community. In his regular podcast series, Goel explained everything from contact tracing to the process for developing a vaccine.
“Our goal is to help make sense of the complex and often conflicting messages about COVID-19 that are bombarding Canadians,” he says.
As the COVID-19 crisis enters the vaccination phase, Goel, too, will be entering another phase of his remarkable career: as president and vice-chancellor of University of Waterloo, beginning July 1, 2021.
U of T President Meric Gertler thanked Goel for his years of distinguished service and wished him well in his new role. “Vivek has made extraordinary contributions to U of T’s success, to higher education and advanced research more generally, and to public health and public policy. We are deeply grateful for his leadership and his friendship, and I look forward to collaborating with him as a fellow president of one Canada’s U15 research universities.”
COVID-19 and Epidemiology
DLSPH epidemiologists have been at the forefront of the statistical work on COVID-19 since the start of the pandemic.
Researchers based at the University of Toronto’s Institute for Pandemics (IFP) – including DLSPH Prof. David Fisman and Assoc. Prof. Ashleigh Tuite, collaborated with Markham-based Scarsin Corporation to advise on and support the deployment of pandemic response tools and technology. The collaboration’s initial focus has been on supporting pandemic forecasts at the federal and provincial levels, built up from local health regions, including building scenarios that could inform the planned 2021 vaccination program.
Fisman and Tuite also created a disease-transmission model early in the pandemic that demonstrated that the start of the pandemic in China likely occurred earlier than reported, based on the mathematics behind the spread of the disease. The site replicates epidemiological scenarios using open-access data that Profs. Tuite and Fisman update daily and allows people to visually and numerically grasp how different scenarios can alter the trajectory of the disease.
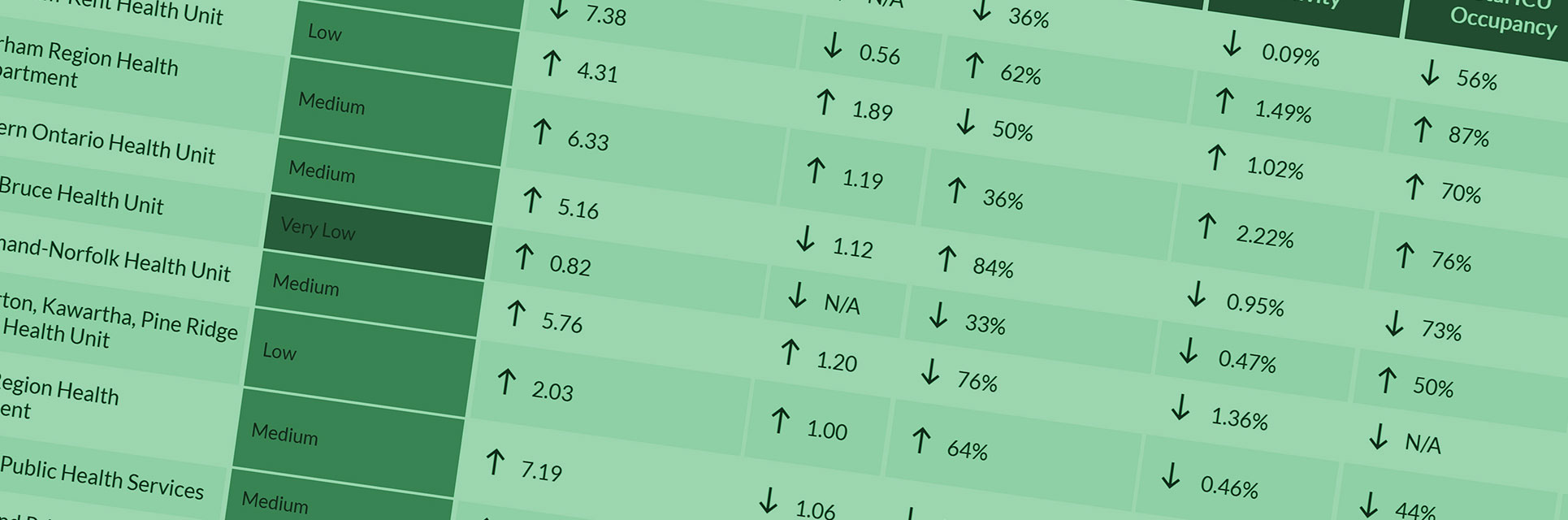
Prof. Laura Rosella is a driving force behind the much-lauded How’s My Flattening website, a COVD-19 site that provides each Ontario resident with tailored pandemic information focusing on their own neighbourhoods to learn about new cases and percent positivity, testing turnaround times and risk levels.
“The ability to provide local insights can both contribute to understanding spread as well as inform more precise mitigation strategies,” says Rosella, an expert in Big Data and Artificial Intelligence.
Meanwhile, Susan Bondy, an associate professor at DLSPH, has been one of the public experts who regularly explains various aspects of the data about COVID-19 to the general public through the media.
COVID-19 and Equity
COVID-19 has magnified socio-economic inequities in Canada, and DLSPH faculty are at the forefront of change.
Roberta Timothy, an assistant professor with DLSPH’s Institute for Pandemics, is launching a nationwide study of the impact of the COVID-19 pandemic on racialized communities as well as existing biases in the health-care system. Timothy’s project will collect data about how Black people interact with the health-care system and will explore economic impacts, evictions, support networks and essential work being done by marginalized communities.
“An underlying part of the project is not only to bring better data, but to support the community in strategizing and finding interventions to find how we get through this,” Timothy tells the CBC.
Arjumand Siddiqi, Canada Research Chair in Population Health Equity and head of the DLSPH Division of Epidemiology, has strongly argued for a better understanding and response to the inequities underscored by the pandemic. She has explored the data and come away dismayed by what she sees: a segregated city whose essential workers – most likely to be exposed to COVID-19 – are largely non-white. They are the ones who work tirelessly in long-term care homes to care for the vulnerable population of seniors, often forced to take risks on public transit because the affordable neighbourhoods aren’t in the city’s core.
COVID-19 and Homelessness
The COVID-19 virus has laid bare the public health implications of homelessness and long-standing systemic inequalities. This spring, IHPME assistant professor Dr. Andrew Boozary and Faculty of Medicine lecturer Dr. Andrew Bond teamed up with Angela Robertson, executive director of the Parkdale Queen West Community Health Centre, to create Toronto Region’s COVID Homelessness Response. Their initial work established spaces for the homeless population to isolate and recover if they, or a close contact, tested positive for COVID-19.
Organizers of the Homelessness Response provided a GTA hotel room for each person or family. During the first wave, 1,000 people (of the 5,000 assessed) received on-site access to health and social care. Staff also ensured that everyone had a primary care provider by the time they left these recovery centres.
A Pandemic Course Taught During A Pandemic
When COVID-19 hit Canada full force, Blake Poland, an associate professor in the Social and Behavioural Health Division, saw beyond the crisis to an opportunity to teach a course about the pandemic in real. Within days, he and colleagues Erica Di Ruggiero, Andrea Cortinois and educational technologist Obadiah George had 24 guest speakers lined up – including some who offered video segments direct from the front lines.
Rather than simply focusing on infection control and policy, Poland chose to address other dimensions of the “battle,” such as the impact on marginalized communities and ethics. Poland has long sought to create spaces for different viewpoints in public health academia. He saw the emerging epidemic, without an established narrative attached to it, as fertile ground for such discussions.
Research Into Lab Testing and Workplace Reopening
When it became clear that Canada urgently needed innovative, made-in-Canada solutions to protect workers and citizens from COVID-19, Prof. James Scott and his team from the Occupational & Environmental Health Division of DLSPH put their lab to work.
Canada didn’t have facilities to test masks and techniques to decontaminate them, but Scott and his team were already experts in aerosol testing with high-end research equipment. Although the lab was not designed specifically for these testing purposes, the team quickly adapted and got to work.
The lab began testing all kinds of masks, with a heavy focus on testing hospital decontamination processes for the N95. Scott’s team was also involved in validating the full-face snorkel mask (an alternative to the N95) developed at Sunnybrook Hospital. They’ve acquired new students to meet the surge in demand and breadth of support needed during the pandemic, and doubled their lab’s testing capacity.
Scott also collaborated with assistant professor Victoria Arrandale, an occupational health expert at DLSPH, to co-create Canada’s first comprehensive report on workplaces safely reopening after the first wave. The pair, along with Associate Dean France Gagnon, DLSPH occupational, students, colleagues and the Canadian Standards Association, developed these return-to-work guidelines as a way of safely getting the Canadian economy rolling again. This meant looking at COVID-19, but also at other potential threats posed by building that had been closed for a few months, such as Legionnaire’s Disease. The report combines research and statistics with a practical guide.
7 IHPME


I’m looking forward to continuing to work with such a multidisciplinary and innovative group of researchers and to help propel the Institute forward as we make our mark globally.
The Institute of Health Policy, Management and Evaluation (IHPME) integrates application of cutting-edge theory and methods to better understanding of health and health systems questions. The Institute’s exceptional faculty and student scholars engage with health care professionals and policy makers across health and social care to enhance the sustainability, performance, and equity of health systems with the goal of advancing population health. The work of the Institute has been particularly noteworthy and central to the public health-care system during the 2019–2020 academic year.
New Leadership
There is much to report about IHPME’s achievements during the ever-changing landscape of this past academic year, not the least of which was the appointment of a new director, Professor Audrey LaPorte. Laporte began her five-year term in January 2020.
Professor Laporte is an internationally recognized scholar with expertise in dynamic microeconomic theory, applied labour economics and econometrics. She has been a faculty member of the Institute since 2001, recently serving as the Program Director for the Health Services Research Program and as the Institute’s Interim Director since June of 2019.
“I’m looking forward to continuing to work with such a multidisciplinary and innovative group of researchers as Director, and to help propel the Institute forward as we make our mark globally,” Laporte says.
Professor Laporte received another honour this year when she was named President-Elect by the International Health Economics Association, one of the world’s largest and most prestigious health economics associations. She is one of only a few women to undertake this role, as well as the first Canadian.
“To me it shows that insights from the Canadian policy environment are contributing to a broader international discussion and is a reflection of the high-quality analysis being done in a multi-disciplinary environment such as IHPME,” said Laporte.
New faculty members continued to enhance the roster of talented public health professionals who teach and conduct research at IHPME. Meena Andiappan, who teaches organizational behavior in the Health Services Research program, joined IHPME from Montpellier Business School in France. Andiappan’s research has centered around ethical behavior, including ethical leadership and change mechanisms.
Andiappan expressed her pleasure at joining IHPME, saying, “The Institute is so interdisciplinary, bringing together people from different types of educational backgrounds, and I find that the best research often comes from this kind of collaboration—where each person shares and leverages their expertise to shed new light on challenging questions.”
Kerry Kuluski, a status Associate Professor at IHPME, has taken on a new challenge as the Dr. Mathias Gysler Research Chair in Patient & Family Centered Care and Scientist at Trillium Health Partners Institute for Better Health. Kuluski will focus on creating a measurement strategy to capture the things that matter to patients and families in their care. Closely connected to that is optimizing care experiences, particularly as patients and caregivers transition from one area of care to another, while also considering the needs of providers and decision makers.
“The Institute for Better Health is a known innovator, unafraid to test out new models of care,” said Kuluski. “They also stand behind a learning health system approach, and it’s what sets them apart. Having researchers work closely on the front line to understand what is needed, and trying new things as they go, is part of the constant learning cycle.”
She joins IHPME Professors Robert Reid and Walter Wodchis, who are also faculty at the Institute for Better Health. Reid is the Institute’s Chief Scientist and the Hazel McCallion Research Chair in Learning Health Systems. Wodchis is the Research Chair in Implementation and Evaluation Science.
Professor Julia O’Sullivan joined IHPME in June 2020. A former dean of education at U of T, Western University and Lakehead University, O’Sullivan’s research and development work are focused on children underserved in schools, especially their inherent right to be taught literacy skills.
Partnerships
The collaborative endeavours undertaken by IHPME faculty members demonstrated the DLSPH commitment to one of the goals of the School’s 2019–2024 Academic Plan: Creating a global presence through collaborative research and education in health system strengthening with a focused set of strong partners.
For example, the North American Observatory on Health Systems and Policies (NAO), under the leadership of Professor Greg Marchildon and associate professor Sara Allin, partnered with WHO to reliably track and document the policy interventions by federal, provincial and territorial governments in response to the COVID-19 pandemic and to make that information publicly available. The NAO team has created a detailed policy timeline that outlines the timing and severity of policy and public health interventions to mitigate the impact of COVID-19.
“By creating a credible, open resource that captures the timing, intensity and range of measures taken across Canada, we’re providing indispensable support to decision-makers across the globe who are navigating COVID-19 policies,” said Allin, who is Director of the NAO .
Meanwhile, Professor Vivek Goel and Julie Zarb, an assistant professor in IHPME’s teaching stream, led the secretariat for a platform that brings together more than 2,500 researchers from across the country to provide the federal government with the best evidence to inform COVID-19 policy-making. As Goel takes up his new role as President of the University of Waterloo, IHPME Professor Peter Jüni will transition into the leadership of the CANCOVID initiative.
“COVID-19 is sparking new demands on health system leaders and the surge of need is bigger than traditional communications can carry,” says Zarb.
Professor Fiona Miller, IHPME’s chair in health management strategies, formed a partnership with the Centre for Sustainable Healthcare (CSH) in the United Kingdom and launched the Centre for Sustainable Health Systems with a vision of creating “health systems characterized by practices and policies that are environmentally, socially, and financially sustainable, allowing us to address the health and care needs of today without compromising our ability to address those needs tomorrow.”
“Once you see sustainability as a dimension of quality, it shifts thinking among health system professionals and encourages mobilization. I wanted to infuse that energy into what already exists here at IHPME, which is this constant drive to improve our health system,” said Miller. “As a Centre, our goal is to work in collaboration with a growing number of clinician leaders, healthcare managers and health researchers who are concerned about these issues, and through partnerships with organizations in the health sector, to encourage and support sustainable health system change, through education, research, and service-oriented action.”
NON-COVID-19 RESEARCH (Read about COVID-19 research)
Although many health-care researchers directed their energies toward pandemic-related research this past year, there were other significant papers published by IHPME faculty, students and alumni.
Cost of Adverse Events
Researchers from the Institute of Health Policy, Management and Evaluation, used a data tool developed by the Canadian Institute for Health Information (CIHI), and the Canadian Patient Safety Institute (CPSI), to estimate, for the first time, the impact of hospital harm on Ontario’s health system, and the striking result is a cost upwards of $1 billion and close to 408,000 additional hospital days.
“Experiencing harm in hospital can extend your stay, which is well-established, but what is novel about our study is that we show that its impact extends to post-discharge health services utilization and estimate the total health system impact of that harm on our resources,” said Lauren Tessier, lead author of the study and a PhD student at IHPME.
Tessier and her fellow researchers measured the occurrence of hospital harm within patient-centered episodes or PCEs, a methodology that was only recently developed by IHPME associate professor Sara Guilcher, who is also a co-author on this study. The research was published in the Canadian Medical Association Journal.
Free Medication and Adverse Health Outcomes
Nav Persaud, an associate professor at IHPME and a clinician-scientist at the Li Ka Shing Knowledge Institute of St. Michael’s Hospital, led a study that found that distributing essential medicines at no charge to patients resulted in a 44 per cent increase in people taking their medications.
“It is sad that in a high-income country like Canada, millions of Canadians cannot afford their prescribed medications—including life-saving medicines such as insulin,” said Persaud. “We hope that our findings help inform public policy changes. This is no longer a question of whether free distribution of medicines can improve health outcomes. It is a question of whether governments will act.”
Immigration and Health
A study led by IHPME graduate Ghazal Fazli, who earned her PhD at U of T, found that immigrants to Canada have a 40% higher risk of developing prediabetes compared to long-term residents. The study, published in BMC Medicine, also found that young adults of South Asian descent develop prediabetes 15 years earlier than those of Western European descent.
“This is a significant finding because our current guidelines recommend screening all adults for type 2 diabetes at age 40. Yet there is evidence that those of South Asian descent are at a much greater risk at of developing prediabetes much younger age,” said Fazli. “Theoretically if we identify someone’s risk earlier, we can provide them with an opportunity to adopt lifestyle changes. This could decrease their risk of developing type 2 diabetes by nearly 60% according to randomized trials, but if we don’t identify them early, they enter the system too late and at a greater cost to the health system.”
Student Research
IPHME’s students are the future of our public health care system and will contribute to policy and practise, not only in Canada, but across the globe. We are proud of all of our students, but we specially commend those students and graduates who earned awards and external recognition this past year, as well as those whose initiatives made a real contribution to public health.
A Case for Revising Cancer Screening Guidelines
Jill Furzer and Lauren Tessier, PhD students at the Institute of Health Policy, Management and Evaluation, led a study showing that early mammographic and MRI screening for female survivors of Hodgkin’s lymphoma (HL) is a costly strategy that provides very limited additional benefits in preventing cancer compared to having an MRI alone.
Furzer and Tessier found that screening with both an MRI and mammogram at age 30 is on average more expensive and less effective than screening using MRI only. They also found that at age 25, adding an MRI to mammography screening also added significant costs without a meaningful change on life expectancy or quality of life for the survivor.
“Mammograms are not as sensitive as MRI in their ability to look for new tumors, especially in women under age 50, and there is often a low compliance rate in this population of women,” said Tessier. “Our findings show that the guidelines should be more specific to an individual’s specific risk profile and that survivors of pediatric HL would likely benefit from starting screening earlier than age 30.”
Seeing Barriers Clearly
Afua Oteng Asare, a PhD student at the Institute of Health Policy, Management and Evaluation, has been analyzing the cost-effectiveness of the Ministry of Health and Long-term Care’s recent child vision protocol. As part of Ontario’s public health standards, health units are now required to provide vision screening in all kindergarten classrooms.
It is a concern that requires attention, noted Asare, because vision screening is key to diagnosing two very common and major conditions that often begin in childhood: refractive errors which include short-sightedness (myopia), long-sightedness (hyperopia), and blurred vision near and far (astigmatism).
Asare has been interested in examining barriers to vision care access since she first began her clinical practice as an optometrist in Ghana. She saw that most patients coming to have their eyes examined were of a higher socio-economic status and began to question how it might be possible to make vision care accessible to everyone.
Improving Sleep
Stuart Douglas, an Emergency Physician and Intensivist and recent graduate of the Master’s in Quality Improvement and Patient Safety (QIPS), at IHPME has developed a quality improvement initiative at Kingston Health Sciences Centre that promotes better sleep for patients in the ICU.
“After admission to the ICU patients are often at risk of developing post ICU syndrome, which comes with a constellation of functional limitations that can last a lifetime,” said Douglas.
Some of these limitations for patients are physical, involving decreased work capacity and muscle fatigue, while other symptoms are neuro cognitive and can include a range of psychiatric issues. Improving sleep may mitigate the risk of developing these issues.
Douglas’ project earned him the Harry and Rose Perlstein Award, presented to a student whose research has the potential to improve health care services for patients in long-term and acute care settings
Venturing into the World of Podcasting
Matthew Goulbourne and Sarah Sawaya, of the Master’s in Health Administration program, launched a podcast about emerging health leaders called Built to Lead. The show is based on leadership concepts shared at Vernissage Health, a dialogue series that pairs IHPME graduate students with established health-care leaders.
The pair wrapped up a successful, six-episode inaugural season, the theme of which is “Leadership: From Self-doubt to Confidence.” They capped the season with a live webinar on Oct. 1, 2020 featuring Matt Anderson, CEO of Ontario Health, and Camille Orridge, former CEO of the Toronto Central LHIN and a senior Fellow at Wellesley Institute.
Sawaya notes they had to wear many hats: technician, producer, host, editor and marketer. She found interviewing guests particularly rewarding. “I think we both improved our communication skills a lot. If you listen from the first episode to the last episode, you can see the difference. I use those skills every day at work. It was one of the only things I’ve done where I can see the direct one-to-one value,” she says.
The podcast can be found on all major streaming platforms.
Leading a COVID-19 Effort
As the pandemic unfolded, students in IHPME’s System Leadership and Innovation (SLI) program stepped up and demonstrated – no real surprise – leadership with initiatives that provided public information and assistance.
A team of SLI students, including Ushma Purohit, Daniel Lee, Monisha Persaud and Geoffrey Sem, developed the COVID19 Central website, an online hub of news and resources that simplifies access to information for the general public as well as for health-care providers. A separate team, that also included Purohit, launched a site called COVID19Ask. This website provides well-researched and expert-verified answers to the most frequently asked questions regarding COVID-19. The information on the site is reviewed by a team of infectious disease experts, physicians and epidemiologists.
Lee is one of 270 students taking part in the Student-Senior Isolation Prevention Partnership (SSIPP), an ongoing initiative that pairs students with socially isolated older adults in the community to provide weekly phone check-ins to promote social connection and improve health literacy of COVID-19. The volunteers are also teaching seniors to use technology, assisting with grocery delivery, and developing a FAQ for seniors regarding COVID-19 and relevant community resources.
And, during March Break, he recruited more than 500 student volunteers from medicine, public health, nursing, social work, and other health faculties to support health professionals with these day-to-day tasks. Lee co-led a steering committee that matched student volunteers with health-care professionals on a one-on-one basis.
“I think all of us were seeing our preceptors and instructors going to the front lines and we want to help out as much as we can,” said Lee, a second-year SLI and U of T Medicine student.
Notable Student and Alumni Awards
- Eleven IHPME students received Vanier Canada Graduate Scholarships in 2020. The scholarships are among the most prestigious and competitive graduate awards. Vanier scholars are recognized for their academic excellence, research potential, and leadership and receive $50,000 of guaranteed funding support for three years during their doctoral studies. IHPME’s 2020 awardees are Federico Angriman, Danielle Baribeau, Doug Cheung, Karen Chung, Erik Friesen, Victoria Haldane, Ayah Nayfeh, Jill Macklin, Hala Muaddi, Chris Noel and Sahr Wali.
- Four IHPME students were among the master’s degree students across the country to receive Vector Scholarships in AI. Michael De Wit, Rachelle Perron, An-Qi Shen and Jamie Wang were nominated by program director Julia Zarb for their vision and drive in their efforts to support AI development across Canada and within the health system. The Vector Scholarship in AI recognizes promising AI talent and supports recruitment of top students to AI-related master’s programs in Ontario.
- Marnie Howe, a graduate of IHPME’s MSc in Health Administration program, was selected as U of T’s annual recipient of the Robert Wood Johnson Award, given to six Canadians who have made promising contributions to health services management and plan to continue working in the field. As a physician, Howe has made it her goal to advocate for palliative care supports for patients at their most vulnerable. She worked as the home care lead physician for the Temmy Latner Centre for Palliative Care based out of Sinai Health System, before assuming her current role as the physician lead for special projects within Medical Affairs at Sinai Health Systems, thanks in part to her practicum placement during MHSc program.
- Fahima Dossa’s timely research has earned her the prestigious Royal Society of Canada Alice Wilson Award, named in honour of the first woman elected to the Royal Society in 1931 and given to three women researchers from across Canada. The award recognizes Dossa’s outstanding academic achievement and her continued work as a postdoctoral researcher on issues facing women’s health care. During her PhD studies, the IHPME graduate in health systems research sought to understand the health care decisions that women make, specifically those who undergo genetic testing for the BRCA1 and BRCA2 mutations, to determine their risk of breast and ovarian cancer.
In Memoriam: Dr. Peggy Leatt
IHPME also experienced loss this year with the death of Peggy Leatt, former chair of the Institute of Health Policy, Management and Evaluation. Recruited by the University of Toronto in 1980, she served as chair of IHPME from 1988–98. Leatt was a respected educator and a leader in the field of health management. She was the first woman to chair the Board of the Association of University Programs in Health Administration (AUPHA) and the first Canadian to chair the Board of the Accrediting Commission on Education for Health Services Administration Commission (now CAHME)—two international leadership roles in improving health care education.
8 Stats
DLSPH at a Glance
DLSPH is the largest and most comprehensive public health school in Canada. As of April 2020, we have:
Faculty
- 88 Core Faculty
- 63 Cross-Appointed Faculty
- 618 Status Only
- 249 Adjunct
- 15 Canada Research Chairs
- 7 Promoted to Associate Professor
- 6 Promoted to Professor
Staff
- 166 Research
- 48 Admin
- 31 Post-Doctoral Fellows
Students
- 837 Master’s Program Students
- 354 PhD Program Students
Annual Research Funding
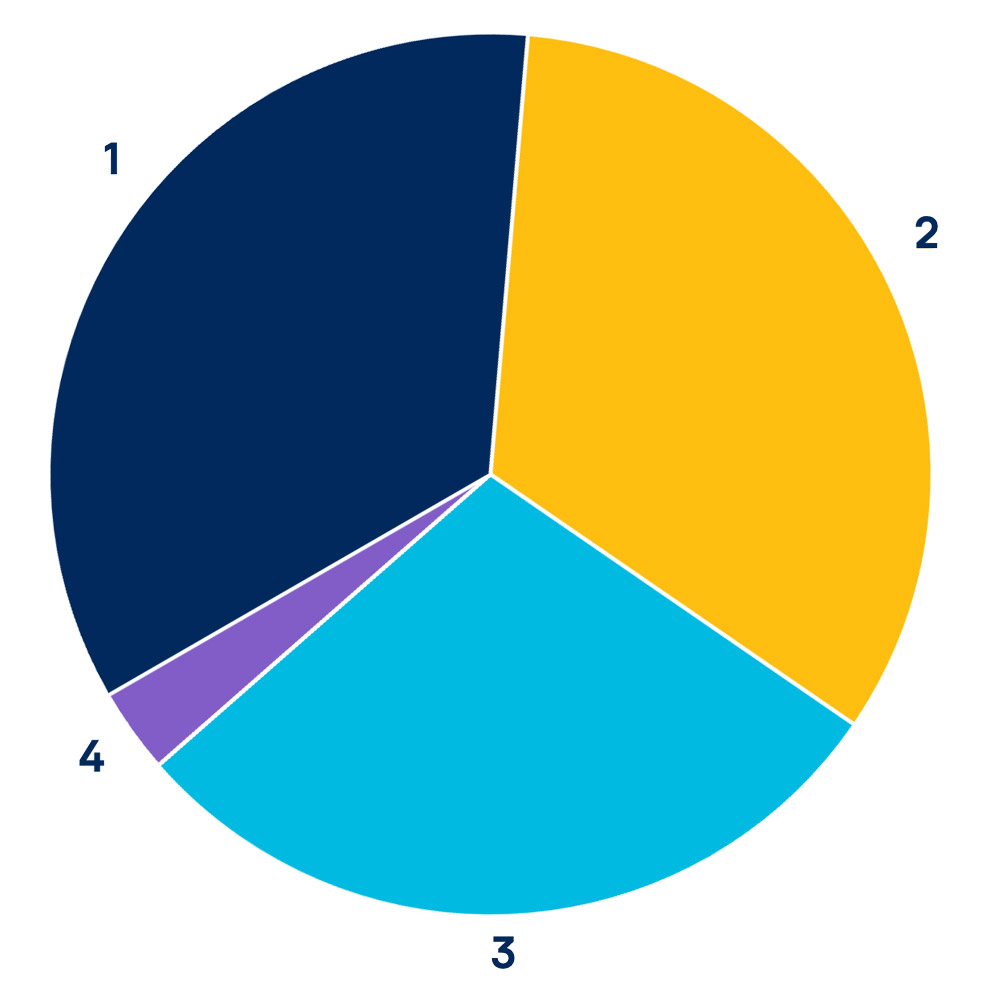
$53,302,752 of total funding, an increase of 60% from 2014-2015.
- 1 Not for Profit | $19,007,689 (36%)
- 2 Three Councils | $18,619,863 (35%)
- 3 Government, Other | $11,944,668 (22%)
- 4 Private, Other | $3,730,532 (7%)
September 2019 Intake
Public Health Sciences (Domestic)
| PhD | MPH | MSc | MScCH* | MHSc | |
|---|---|---|---|---|---|
| Applications | 155 | 863 | 171 | 105 | 25 |
| Offers | 37 | 215 | 67 | 68 | 16 |
| Registrations | 27 | 135 | 36 | 49 | 11 |
*Master of Science in Community Health
Institute of Health Policy, Management and Evaluation (IHPME)
Academic Year 2019-2020
| PhD | MSc | MHSc Health Admin |
MHI* | Exec. MHI |
|
|---|---|---|---|---|---|
| Applications | 90 | 255 | 145 | 214 | 40 |
| Offers | 39 | 127 | 48 | 45 | 32 |
| Registrations | 36 | 112 | 43 | 36 | 27 |
*Master of Health Informatics
2019-20 Annual Report
Writing: Elaine Smith
Design: Andrew Munroe